Diabetes and elevated blood glucose levels cause blood vessel damage throughout the body. The damage is most severe to small blood vessels, especially the eye, kidney, fingers and toes, heart, and brain. As long as the blood glucose is elevated, microscopic damage to the cells that line the walls of small blood vessels and microaneurysms form. These are focal areas of weakness in the walls of the blood vessels that can then bleed or leak fluid and lipid into the retina as the earliest signs of diabetic retinopathy.
The beginning stages are known as Non-Proliferative Diabetic Retinopathy (NPDR) and are graded based on severity; mild, moderate, and severe. As the damage progresses, the vessels in the periphery of the retina become unable to carry blood to supply the nutritional needs of the retina. Eventually, the retina responds with the development of new blood vessels, a process known as neovascularization.
Proliferative Diabetic Retinopathy refers to new vessels forming in the retina. Diabetes damage accumulates over a lifetime and does not result from one short period of elevated blood glucose. Consequently, most people will develop some diabetic retinopathy in their lifetime .
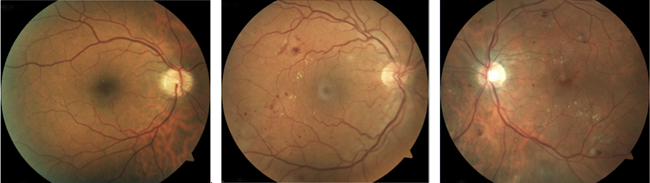
Mild, moderate, and severe Non-proliferative Diabetic Retinopathy
Since diabetic retinopathy occurs due to chronically elevated blood glucose, controlling blood glucose is essential to preventing vascular damage. Keeping blood glucose levels below 120 mg/dL and Hemoglobin A1C at 6.5% dramatically reduces the risk of developing retinopathy. Additionally, controlling underlying hypertension minimizes the amount of vascular damage.
We recommend that all patients with diabetes get routine, dilated eye exams to check for retinopathy. Since Type 1 diabetes present suddenly, screening is performed within five years of a diagnosis. Type 2 diabetes, however, may have been present for an extended period before diagnosis. The initial stages of diabetic retinopathy typically do not have any symptoms, making periodic screenings critical.
The screening exam consists of a complete, dilated examination of the eye and retina. The amount of diabetic retinopathy and risk for vision loss is assessed by carefully looking at the retina. If any complications are present, they can be detected and properly treated. Optical Coherence Tomography (OCT) is a retina scan, often performed to examine the retinal structure. OCT is beneficial for assessing macular edema. The measurement follows the response to treatment. Sometimes a Fluorescein Angiogram (FA) is performed. This test uses a special dye to check the blood flow in the retina and identify areas of leakage.
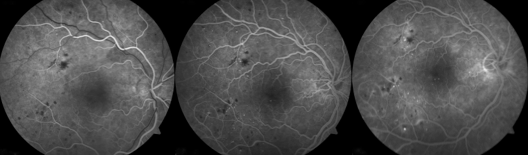
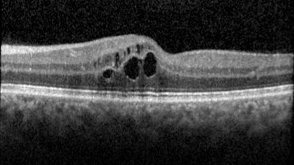
If microaneurysms are present in the central retina, the macula, the leaking fluid, and swelling can lead to decreased vision called Diabetic Macular Edema. Since the macula is responsible for central vision, a small amount of damage can cause a significant decrease in vision.
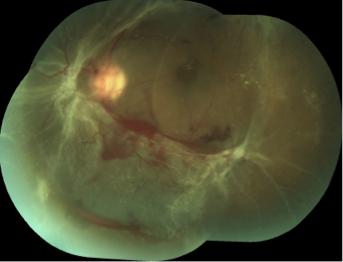
In proliferative diabetic retinopathy, neovascularization can lead to bleeding that fills the inside of the eye, causing decreased vision, known as Vitreous Hemorrhage.
Neovascularization in PDR can also lead to scar tissue development, and if it progresses without control, it can pull on the retina and cause a Tractional Retinal Detachment. This complication of diabetic retinopathy is severe and leads to complete blindness.
Neovascularization can occur in the front of the eye and the retina and can block the normal fluid drainage network of the eye, causing elevated eye pressure, termed Neovascular Glaucoma (NVG). NVG results in elevated intraocular pressure and sudden bleeding in the front of the eye, resulting in severe eye pain and redness. If the eye pressure is not controlled, there can be a complete and irreversible vision loss.
Neovascular Glaucoma
Standard therapy for Macular Edema includes treating the microaneurysms with Focal Laser Photocoagulation to seal the leaking areas. While effective, patients can have a variable treatment response, and the laser has the risk of causing damage to the surrounding retina.
More recently, injectable pharmacologic agents block Vascular Endothelial Growth Factor (VEGF), a molecule in the eye that leads to increased vascular permeability. These agents are bevacizumab (Avastin), ranibizumab (Lucentis), aflibercept (Eylea), and antibodies against the VEGF molecule. Lucentis and Eylea are FDA approved for the treatment of diabetic macular edema, while Avastin is not. These Intravitreal medications are injected directly into the eye and are effective for 4-6 weeks.
Response to the medicines varies. There is no way to predict how many treatments will be necessary. In some patients, response to anti-VEGF molecules is inadequate. In this case, steroids are injected into the eye or next to the eye to control the vessel leaking. Triamcinolone is the most common steroid used, and the FDA has approved Ozurdex (dexamethasone), an implant that can slowly release steroids for up to 3 months.
When the peripheral retina does not receive adequate blood supply from the damaged vessels, it begins forming abnormal blood vessels, known as neovascularization. The retina causing the neovascularization is significantly damaged from ischemia and does not function for vision. Unfortunately, there is no way to undo the damage or restore the blood flow, and laser photocoagulation is used to burn this retina, termed Pan-Retinal Photocoagulation (PRP).
After PRP, the nutritional requirement of the peripheral retina is decreased, and once the balance is achieved between the retina and blood supply, the neovascularization process will stabilize. Sometimes only one laser session is needed, but often multiple sessions are required to control the disease. If diabetes damage worsens from continued uncontrolled blood glucose, we might repeat treatment in the future.
When the eye has bleeding from neovascularization, it prevents light from passing through the eye and causes decreased vision. Mild bleeding will cause floaters or strings in the vision, and very dense bleeding can cause significant vision loss. With enough time, the blood will be broken down and absorbed by the eye, but the underlying cause of the bleeding must be treated. If the bleeding is not severe, Pan-Retinal Photocoagulation (PRP) treatment can be applied through the blood in the clinic to control the underlying disease, and then the vitreous hemorrhage can be safely monitored as it clears.
If the bleeding is too dense to apply PRP in the clinic, the blood is removed during a surgery known as Pars Plana Vitrectomy (PPV). A PPV is performed in the operating room under sterile conditions and involves making small incisions in the eye, using specialized equipment to remove the blood and the vitreous gel that fills the eye. A PRP laser is applied during the procedure to stabilize the diabetic retinopathy.
If scarring along the retina becomes severe, the traction can pull the delicate retina and cause separation from the wall of the eye. Severe scarring is very damaging to the retina and can result in significant vision loss. If the retinopathy is stabilized with Pan-Retinal Photocoagulation (PRP) treatments, the scarring may stop. Still, it will not reverse itself, and a Pars Plana Vitrectomy (PPV) may be required to remove the scar tissue and repair the retina.
Under a microscope with high magnification, the scar tissue is delicately separated from the retina and releases the traction allowing the retina to reattach to the wall of the eye. PRP treatment is applied simultaneously to ensure that the underlying retinopathy is stabilized. Often the retina will need internal support during the healing process, with an intraocular gas bubble deployed to allow it to heal. If a gas bubble is necessary, then the head and eye will need to be positioned face down toward the ground to allow the gas bubble to support the retina. Sitting in a facedown chair (such as a massage chair) may be necessary for several weeks after surgery.
The same process that causes neovascularization of the retina can cause neovascularization of the iris. These blood vessels can block the eye's normal drainage network, causing fluid buildup in the eye and elevating eye pressure. Sudden high internal pressure causes significant eye pain and damage to the optic nerve that carries the signal from the eye to the brain. This damage is irreversible. Control of both eye pressure and retinopathy is necessary. Medication, known as bevacizumab (Avastin), is injected into the eye to block the signal that causes blood vessel growth to control neovascularization initially. It will cause the abnormal blood vessels to stabilize and regress. The medication is only temporary until Pan-Retinal Photocoagulation (PRP) treatment can be applied.
If the process is early, then the intraocular pressure can normalize. Often, however, the neovascularization results in scarring of the fluid drainage network in the eye and causes persistently elevated pressure. Topical and oral medications may be necessary to control eye pressure. Still, if insufficient, surgery may be required to shunt the fluid out of the eye and is performed by a surgeon specializing in glaucoma surgery.
Request an appointment now