The retinal blood supply comes from a central artery and vein that enter and exit the eye along with the optic nerve. At this point, the vessels begin to branch out to provide nutrition for the entire retina. As the result of systemic diseases, these vessels can be damaged and pre-disposed to occlusion. The vessels can be blocked as they enter the eye, called a central occlusion, or along with one of the smaller branches.
When a retinal vessel becomes occluded, the area of the retina supplied by the vessel will be damaged and cause the vision to decrease. When the blockage affects the vessels in the retina's center, the macula, vision loss is most significant. The onset is typically sudden or noticed upon awakening, is painless, and can worsen over several days. If severe, abnormal blood vessels may form and cause bleeding in the eye that may cause floaters in the vision or high eye pressure that may cause pain.
The most important part of diagnosing vascular occlusion is a thorough examination of the retina through a dilated pupil. To aid in the diagnosis, a scan of the retina is typically performed with Optical Coherence Tomography (OCT); this allows the retina to be seen in cross-section to evaluate any retinal damage better. The OCT scan can also be used to follow the response to treatment by creating detailed retina measurements.
Another important diagnostic test is the Fluorescein Angiogram (FA), which allows the visualization of blood flow through the retina and can evaluate the full extent of the blockage and the presence of leakage and abnormal blood vessels. Many different retinal diseases can present as fluid or blood in the retina. It is important to have a complete exam by an experienced Retina Specialist to ensure the correct diagnosis and treatment.
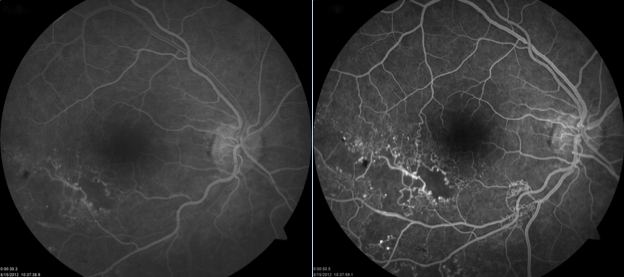
Fluorescein angiogram of retinal vein occlusion shows disruption of the normal blood flow
The retinal veins collect the blood after transferring the oxygen and nutrients to the retina and return it to the systemic circulation. These vessels become blocked due to a clot, or thrombus, forming and preventing flow. Branch retinal veins will occlude at points where they cross the retinal arteries; at these points, the vein narrows, allowing a clot to form. The central retinal vein will occlude as the vein exits the eye with the optic nerve; there is a constriction at this point and can predispose to clot formation. When blood flow through a vein becomes obstructed, the resulting backup causes leaking fluid, bleeding, and poor blood flow. These components can cause vision damage, and while fluid and blood can resorb, poor blood flow causes permanent tissue damage. The amount of poor blood flow, or ischemia, determines the visual prognosis.
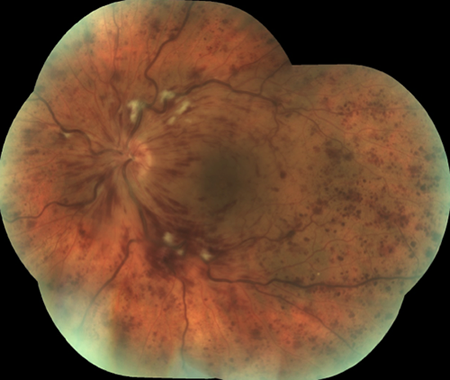
On examination, blood leaks from the damaged veins into the retina
The damage to retinal vessels is the same damage to vessels in the brain and heart that lead to heart attack and stroke. The significant risk factors are the systemic medical problems of hypertension, diabetes mellitus, hyperlipidemia, and smoking. It is essential to work with a Primary Care Doctor or Internist to control systemic factors to minimize risk.
Treatment for BRVO and CRVO is similar and involves controlling the leakage from the damaged blood vessels that lead to edema and limiting the development of abnormal blood vessels as the retina tries to heal.
The leakage from the damaged vessels is driven by inflammation and a molecule secreted due to the tissue damage, vascular endothelial growth factor (VEGF). To combat this, an antibody is injected into the eye by Intravitreal Injection to bind the VEGF molecule and prevent it from stimulating vessel leakage; these medications are known as antiVEGF compounds. There are three drugs currently available in this class.
Using these medications, the leakage can be controlled to improve the vision loss associated with the fluid buildup.
Inflammation also plays a role in blood vessel leakage, and when the edema is not controlled with antiVEGF compounds, steroids may be used. These steroids can be given beside the eye or inside the eye. Triamcinolone is the most commonly used steroid but lasts for a shorter time than a dexamethasone implant (Ozurdex) which can last up to 3 months. The side effects of steroids include glaucoma and cataract formation, which will be monitored and treated if they occur.
Any medication used to treat edema is temporary and must be repeated as long as the damaged veins continue to leak. Treatments and examinations will be individualized and repeated as necessary until the condition stabilizes.
As the retina tries to heal, abnormal blood vessels, or neovascularization, can develop in an attempt to restore blood flow to areas of the ischemic retina. These blood vessels can grow along the retina, optic nerve, or in the front of the eye and the iris. If the vessels grow along the retina or optic nerve, they can lead to bleeding that fills the eye and blocks the vision, known as a vitreous hemorrhage. These vessels can also lead to the development of scar tissue that can pull on the retina and cause retinal detachment. If the blood vessels grow along the iris, the eye's fluid drainage system can be blocked and lead to elevated eye pressure, known as neovascular glaucoma. Often the elevation can be very sudden and severe, resulting in sudden decreased vision and pain.
To control these vessels, laser photocoagulation by Pan Retinal Photocoagulation (PRP) is needed to treat the ischemic areas of the retina. The laser burns the retina and stops it from producing signals that drive the neovascularization. Sometimes, an antiVEGF medication is given before the laser to control the neovascularization until the laser is applied temporarily. After the retina is treated, the blood vessels will stabilize and regress. In patients with neovascular glaucoma, the eye pressure can normalize, but if too much scarring occurs, the eye pressure may require surgery with a glaucoma specialist.
The retinal arterial supply comes from a branch of the ophthalmic artery from the carotid artery. Arteries carry blood rich in oxygen and nutrients to the retinal tissue. Retinal arteries are susceptible to blockages from debris in the bloodstream (i.e., Embolus) or inflammation of the vessel walls.
Emboli are small debris particles in the bloodstream that can come from many sources. In the retinal circulation, emboli are most frequently from carotid artery plaques or the heart. The carotid artery develops plaques in the walls of the vessel due to long-term hypertension, hyperlipidemia, and smoking. These plaques can obstruct blood flow and rupture, sending small cholesterol particles down the circulation that can be large enough to block the central retinal artery or a branch retinal artery. Emboli from the heart most commonly come from the mitral and aortic heart valves. These valves can be damaged by a congenital abnormality, inflammation, or infection. When debris develops on the surface, the valve's motion can send particles through the circulation.

The retina becomes pale when the standard arterial blood flow is blocked
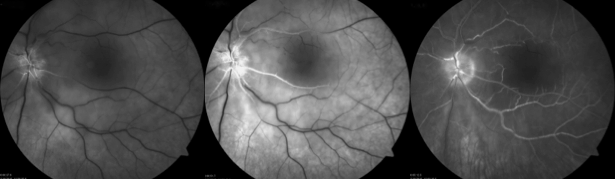
Fluorescein angiogram after retinal artery occlusion shows very poor blood flow to the retina
When retinal arteries are blocked temporarily, there can be a transient vision loss known as amaurosis fugax. The vision undergoes a generalized darkening, graying, or blackening and returns to normal as the blockage resolves and the retina is again perfused with oxygen and nutrients. If the blockage does not resolve, permanent tissue damage can occur after as little as 90 minutes without blood flow. When the central retinal artery is occluded, the entire vision will be affected. A branch artery will affect only the portion of the vision supplied by that area of the retina. After an episode of poor blood flow to the retina from arterial occlusion, the vision loss is permanent and is typically very severe.
After the initial event, the retina will break down the blockage, and blood flow will be restored to the retina, at least in part. However, the vision typically does not improve.
As the eye tries to heal, abnormal blood vessels in the retina or the front of the eye in the iris can develop. This complication needs to be monitored as it can cause additional damage to the retina and the eye. If abnormal vessels develop, laser photocoagulation treatment is necessary to prevent their continued growth.
Treatments are limited in their effectiveness since permanent damage occurs very quickly after the start of symptoms. It is crucial to be evaluated for the cause of the arterial blockage to minimize the risk of further vascular events. Ultrasonography of the carotid artery and an echocardiogram are potential studies that are needed to evaluate the potential cause. Specific blood tests may also be required to assess for a severe systemic inflammation or a clotting disorder. If test results come back positive, it is essential to consider potential treatments. Modifying the risk factors of smoking, hypertension, and hyperlipidemia is critical in reducing the risk of arterial blockage in the other eye and stroke.
Request an appointment now