The central area of the retina is the macula. It is responsible for the central vision and is organized to give the central vision extra sensitivity. A macular hole is a round defect in the central macula and causes a decrease in the central vision as the retinal photoreceptors are disrupted. Sometimes the vision is blurred or distorted, and there can be a visible dark circle.
Inside the main body of the eye is the vitreous gel, and it is adherent to the surface of the retina. As a normal aging process, the vitreous begins to degrade and consolidate, causing it to shrink, liquefy, and eventually separate from the retina. During this process, a mechanical pulling force is applied to the retina, and in some people, this force can be too strong, and a retinal hole can form. Developing a macular hole can happen as a natural occurrence due to the way the eye was made or secondary to another function in the eye, such as trauma or inflammation.
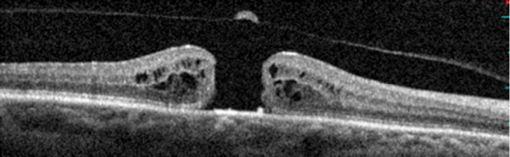
The key to diagnosis is a detailed examination of the retina through a dilated pupil. The macular hole can be seen as a circular defect in the retina. A scan of the retina by Optical Coherence Tomography (OCT) is often performed to characterize the hole better. This allows the visualization of the retina in cross-section and allows for more accurate staging of the hole and the detailed measurement of its size. It is vital that all conditions that can mimic a macular hole and cause macular holes to be evaluated so that potentially more serious diagnoses are not missed.
Macular holes can be categorized based on their level of formation and based on their size.
In these holes, there is still vitreous traction on the retina but with early disruption of the retina.
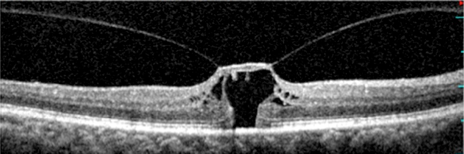
Hole formation but partially relieved retinal traction.
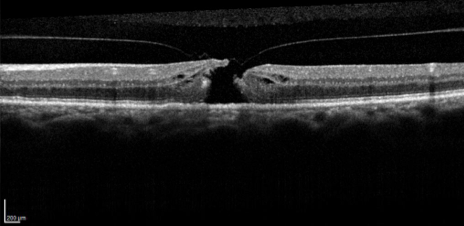
A full-thickness hole has formed with the separation of the vitreous from the macula, but a complete vitreous detachment has not yet formed.
Full-thickness hole with complete vitreous detachment.
A comprehensive exam can determine the difference between Stage 3 and Stage 4 macular holes.
Macular holes are also categorized based on their size:
In cases where the macular hole has vitreous traction, ocriplasmin (Jetrea) is available. Ocriplasmin is an active enzyme injected into the vitreous and breaks down the vitreous gel causing the traction to release. While closing macular holes is not the primary indication of ocriplasmin, it was successful in about 40% of these select cases.
In other patients, the treatment for a macular hole is surgery. The Pars Plana Vitrectomy (PPV) procedure is performed in the operating room under sterile conditions. Small incisions are made in the eye, and, using a microscope for viewing, tiny instruments are used to remove the vitreous gel that fills the inner eye. If any epiretinal membrane tissue is present, it is removed from the retina's surface, and the innermost layer of the retina, the internal limiting membrane, is also removed with the help of a special dye to improve visualization. At the end of the surgery, the fluid is removed from the eye, and it is filled with a special gas that occludes the retinal hole and allows it to close.
To maximize the success of the surgery and the effect of the gas bubble, the eye needs to be positioned looking down to allow the bubble to float up directly on the macula. Depending on the specific circumstances, the face-down position may be required for 3-7 days after surgery. This time is critical for retinal healing and successful surgery. The gas bubble is slowly reabsorbed over several weeks and is replaced with the eye’s natural fluid. When the gas is in the eye, the vision is inferior as light cannot pass through the bubble. The vision improves when the gas resorbs, but the overall visual recovery can take several months as the retinal cell’s function improves.
Pars plana vitrectomy with intraocular gas has a success rate of over 90% in closing macular holes. It is essential to consider that every patient is unique in response to surgery, and certain macular holes may not close even with surgery.
Request an appointment now